Some critical antibiotics now show 79-97% resistance

Several widely used antibiotics in Bangladesh are losing their effectiveness at alarming rates, with resistance ranging from 79 to 97 percent, a WHO report says, highlighting the country's worsening antimicrobial resistance crisis.
Resistance levels of some of these drugs are among the highest in South-East Asian countries, including India, Nepal and Sri Lanka, according to the Global Antibiotic Resistance Surveillance Report 2025, released on Monday.
For example, Acinetobacter spp., the Gram-negative bacteria that can cause bloodstream infections, showed an estimated resistance rate of 97 percent to imipenem, a powerful antibiotic typically applied as a second last-resort treatment for blood infections.
Antimicrobial Resistance (AMR) occurs when bacteria, viruses, fungi and parasites no longer respond to antimicrobial medicines, infections become difficult or impossible to treat, increasing the risk of disease spread, severe illness, disability and death, according the World Health Organization.
Health experts say higher AMR rates can lead to more critical illnesses, prolonged hospital stays, increased treatment failures, greater surgical and medical risks, and ultimately higher mortality.
They warn it would also drive-up treatment costs, increase the burden on healthcare systems, and reduce productivity.
"The latest WHO report echoes concerns highlighted in previous AMR reports released by icddr,b and other government agencies. This is deeply alarming," Dr Gazi Md Salahuddin Mamun, an assistant scientist at the AMR Research Unit at icddr,b, told The Daily Star.
He said the findings of the WHO report are similar to those of an icddr,b AMR study, which monitored patients in hospital Intensive Care Units between July 2023 and January 2024.
Mamun said over-prescribing and overuse of antibiotics, patients not completing their antibiotic courses, overuse of antibiotics in livestock and fish farming, poor infection control in hospitals, lack of hygiene, and poor sanitation are all blamed for the situation.
Prof Halimur Rashid, the immediate past line director of the Communicable Disease Control (CDC) unit at the Directorate General of Health Services (DGHS), said the AMR situation has become very alarming due to the indiscriminate use of antibiotics, which can be easily bought from any pharmacy without prescription.
He added that under the Drug and Cosmetic Act 2023, selling antibiotics without a prescription is strictly prohibited, but the law is rarely fully enforced for a lack of manpower and other challenges.
"The situation will become even more alarming if we fail to stop the indiscriminate use of antibiotics," he told this paper yesterday.
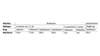
AMR SITUATION IN BANGLADESH
WHO began monitoring AMR in 2015, and released its latest global surveillance report on Monday, based on over 23 million bacteriologically confirmed infections reported by 104 countries, including Bangladesh.
The previous report, published in 2022, did not include data from Bangladesh. The latest report presents WHO's infection data for 2023.
It covers 16 pathogens responsible for four types of infections -- bloodstream, gastrointestinal, urinary tract, and urogenital -- and assesses the effectiveness of seven antibiotics used to treat these infections.
The drugs are: Imipenem, Cefotaxime, Cephalosporins, Ciprofloxacin, Methicilline, Penicillin G and Ceftriaxone. However, Bangladesh data regarding Penicillin G and Ceftriaxone was not available.
WHO classifies antibiotics into three categories -- Access, Watch, and Reserve -- to guide their appropriate use and combat antimicrobial resistance. Antibiotics under Access group should be widely available and used as first- or second-line treatments for common infections.
Antibiotics under Watch group use should be monitored and restricted to specific indications while antibiotic under reserve is the last-resort antibiotics for treating infection caused by multi-drug-resistant organisms.
Of the seven drugs mentioned above, six are from Watch group while Penicillin from Access group.
These drugs show 79 to 96.6 percent resistance in dealing infection caused by five types of pathogens, shows the report.
For example, Cefotaxime shows 79.9 percent resistance in treating bloodstream infections caused by E. coli, while third-generation Cephalosporins exhibit 88.1 percent resistance against the same infection by the same pathogen.
Cefotaxime shows 87 percent resistance in treating bloodstream infections caused by Klebsiella pneumoniae, while Imipenem shows 51.1 percent resistance against the same infections, the report shows.
Ciprofloxacin shows 89.1 percent resistance in treating gastrointestinal infections (that attacks digestive system) caused by Shigella spp while Cefotaxime shows 64.7 percent resistance in treating urinary tract infection caused by E. coli.
In treating at least five pathogens, resistance levels of some of these drugs in Bangladesh are among the highest of 11 South-East Asian countries, the report shows.
All these pathogens can be treated with several drugs, five of which have developed at least 79-97 percent resistance.
For other pathogens, Bangladesh ranks between the second and fifth highest in terms of drug resistance.
At least five pathogens have developed resistance between 16 and 30 percent three pathogens between 51 and 65 percent resistance.




 For all latest news, follow The Daily Star's Google News channel.
For all latest news, follow The Daily Star's Google News channel.
Comments