Cervical cancer: Don't cure. Prevent.
In Bangladesh, 6,582 women die from cervical cancer every year. If the number seems small at first glance, here's another: 11,956 cases get diagnosed annually, while over 58.7 million women (aged 15 or above) are at risk.
The first two figures were found in a study conducted by the International Agency for Research on Cancer (IARC) and the latter was revealed in the Human Papillomavirus and Related Diseases Report (2017). What's astonishing about these numbers is the enormous discrepancy between the cases that get diagnosed and those that don't, a telling sign of the lack of knowledge regarding causes, diagnosis and prevention. "Awareness about cervical cancer is negligible, particularly in low socio-economic groups, who also have the highest exposure to risk. Many don't know about early detection, symptoms, preventive measures or even what cervical cancer is. If they are aware, it's usually a problem that is not prioritised," says Dr Md Habibullah Talukder Ruskin, an Associate Professor and Head of Epidemiology at the National Cancer Research Institute and Hospital.
What stood out from Dr Ruskin's statement is the word "preventive". In fact, upto 93 percent of cervical cancer cases can be prevented, according to a report by the US National Centre for Chronic Disease Prevention and Health Promotion. "The earlier the screening, the higher the chance of averting cervical cancer. Preventive cervical screening programmes are necessary for early detection, which can prevent many cancer-related deaths," confirms Dr Ruskin.
So, how can you prevent cervical cancer? Let's break things down.
What is cervical cancer?
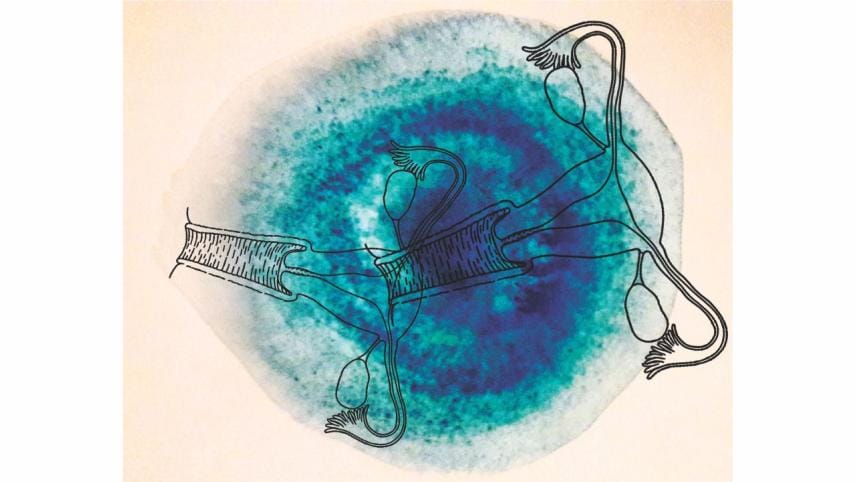
Cervical cancer is an abnormal growth of cells in the cervix, the lower end of the uterus that connects with the upper vagina. Over 90 percent of cases are caused by the Human Papillomavirus (HPV). Most people never even know that they have HPV, as their immune system fights it off. But in some cases, the virus can transform normal cells in the cervix to cancerous ones. Doctors also attribute certain "risk factors" to the likelihood of developing cervical cancer.
When does it occur?
"The occurrence has two peaks, one at about 35 years and another between 50–55 years," says Professor (Brigadier General) Rokeya Khan, MBBS, MCPS, DGO, and FCPS Fellow in Gynae-oncology. "Cervical cancer is one of the most common cancers that occur among women around 35 years of age," confirms Dr Ruskin.
Cervical cancer is the second-most common female cancer in women aged 15–44 years in Bangladesh, according to the 2017 Human Papillomavirus and Related Diseases Report. "While it can develop at any age, the majority of cases tend to occur," explains Dr Ruskin.
Am I at risk?
There are multiple risk factors that increase the probability of cervical cancer, including smoking, HIV infection, long-term use of oral contraceptives, inherited risk, early marriage, lack of personal hygiene (particularly during menstruation), polygamy, STDs, intercourse at a young age (below 16 years) and early and multiple pregnancies. According to Dr Ruskin, the risks are much higher among those affected by poverty: "Early marriage, multiple pregnancies and lack of hygiene tend to be most concurrent in lower socio-economic groups. These groups don't always have access to proper nutrition, adequate sanitation or even basic healthcare. Moreover, early marriage and multiple pregnancies are prominent within these communities, which worsen the risk for women."
When and how can I screen for cervical cancer?
Screening is the best way to avert cervical cancer as it can detect abnormalities, including precancerous lesions and early cervical cancer.
It does so through two tests: the Pap smear and HPV test. The Pap smear can detect and treat cell changes before they become cancerous or diagnose cervical cancer early when it's easily treatable. The HPV test, on the other hand, can identify infections that can cause cell changes or even cancer.
Among these, the Pap smear is more commonly used, but because of its high price, it's not accessible by poorer communities. Due to this challenge, a cheaper alternative called Visual Inspection by Acetic Acid (VIA) has been in use, though it has yet to be popularised. "In low-income communities, particularly those with poor healthcare resources and facilities, cervical cancer screening can be challenging. Both Pap and HPV tests require trained professionals and well-equipped labs, both of which are costly. In such instances, VIA is highly effective," explains Dr. Ruskin.
"Irrespective of the time of occurrence, I believe cervical cancer can be screened at the age of 21 years. Women aged between 21–65 years should continue to get tested and confidently stop at 65 years, if they have had regular screenings with normal results," says Professor Rokeya Khan.
A few NGOs and government organisations, such as Bangabandhu Sheikh Mujib Medical University, A K Khan Healthcare Trust, and Dhaka Medical College and Hospital, already have screening programmes in place.
Is it preventable by vaccination?
Yes. In fact, vaccination against HPV, a common cause of cervical cancer, can entirely reduce your risk.
The two most effective vaccines for protection against HPV are Cervarix and Gardasil. "Patients below 15 years require two doses in six months, whereas those between 16 and 26 years require three, the second being a month after the first and the third six months after the first," elaborates Dr Khan.
Cervarix costs BDT 2,100, whereas Gardasil costs approximately BDT 3,500 per dose. But Dr Khan recommends Gardasil because of its wider benefits. "Gardasil covers anal cancer and warts of the vulva, besides cervical cancer," she elaborates. Vaccination can be administered in hospitals, vaccination centres and by gynaecologists.
Throughout its ordeal, cervical cancer casts an impossible curse on more than just the victim, through more than one front. While vaccination is preventive, it doesn't cure it. But the financial burden implied, the emotional torment shared, and the inevitable grief borne by countless families can be averted. And that's precisely the point—don't cure when you can prevent.
Mithi Chowdhury is a soon-to-be graduate of the Institution of Business Administration, University of Dhaka, and a contributor for Star Weekend and Shout, The Daily Star.




 For all latest news, follow The Daily Star's Google News channel.
For all latest news, follow The Daily Star's Google News channel.
Comments